How to Treat Chronic Obstructive Pulmonary Disease and Relief Products
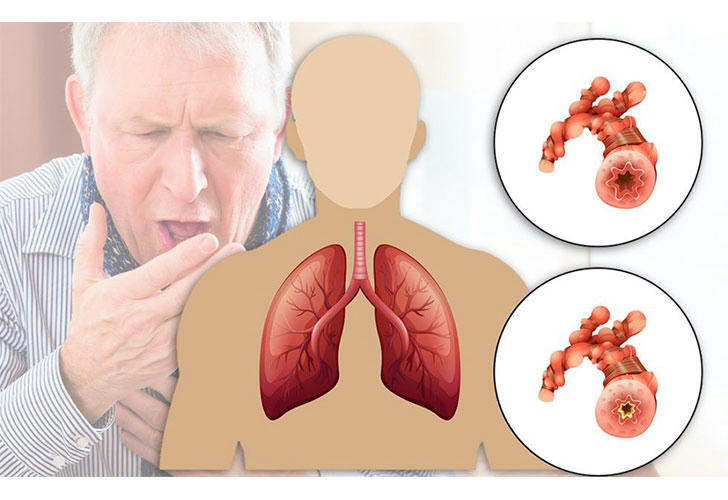
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by persistent respiratory symptoms and airflow limitation. COPD is primarily caused by long-term exposure to irritating gases or particulate matter, most commonly from cigarette smoke. Other risk factors include air pollution, occupational dust and chemicals, and genetic factors. Symptoms often include shortness of breath, chronic cough, wheezing, and fatigue.It encompasses conditions such as emphysema and chronic bronchitis, which can significantly impact the quality of life. While there is currently no cure for COPD, effective treatments can help manage symptoms, improve lung function, and enhance overall well-being.
Understanding COPD
COPD is primarily caused by long-term exposure to irritating gases or particulate matter, most commonly from cigarette smoke. Other risk factors include air pollution, occupational dust and chemicals, and genetic factors. Symptoms often include shortness of breath, chronic cough, wheezing, and fatigue. As the disease progresses, patients may experience exacerbations—sudden worsening of symptoms that require additional treatment.
1. Medications
Bronchodilators
Bronchodilators are the cornerstone of COPD treatment. They work by relaxing the muscles around the airways, making it easier to breathe. There are two main types:
Short-Acting Bronchodilators: These medications are used as "rescue" inhalers for quick relief of acute symptoms. Common examples include:
• Albuterol (ProAir, Ventolin): Provides rapid relief during flare-ups.
• Ipratropium (Atrovent): Often used in combination with albuterol for enhanced effect.
Long-Acting Bronchodilators: These are taken daily to maintain open airways and prevent symptoms over time. Examples include:
• Tiotropium (Spiriva): A popular choice for long-term management.
• Salmeterol (Serevent): Helps improve lung function throughout the day.
Inhaled Corticosteroids
Inhaled corticosteroids reduce inflammation in the airways and help prevent exacerbations. They are particularly beneficial for patients with frequent flare-ups.
Common Inhaled Corticosteroids:
• Budesonide (Pulmicort)
• Fluticasone (Flovent)
Combination Inhalers
Combination inhalers that contain both a bronchodilator and a corticosteroid provide comprehensive treatment for moderate to severe COPD.
Examples:
• Fluticasone/Salmeterol (Advair)
• Budesonide/Formoterol (Symbicort)
2. Oxygen Therapy
For patients with low oxygen levels in their blood, oxygen therapy can be critical. This treatment involves using supplemental oxygen to ensure adequate oxygenation during daily activities or while sleeping.
Types of Oxygen Therapy:
• Continuous Oxygen Therapy: Used throughout the day and night.
• Ambulatory Oxygen Therapy: Used during physical activities or exercise.
3. Pulmonary Rehabilitation
Pulmonary rehabilitation is a comprehensive program designed to improve the well-being of individuals with COPD. It typically includes:
• Exercise Training: Helps improve physical endurance and strength.
• Nutritional Counseling: Provides guidance on maintaining a healthy diet that supports lung health.
• Education: Teaches patients about managing their condition, recognizing symptoms, and using medications effectively.
• Psychosocial Support: Offers mental health support to cope with the emotional aspects of living with a chronic illness.
4. Lifestyle Changes
Making certain lifestyle changes can significantly impact the management of COPD:
• Quit Smoking: The most crucial step for anyone with COPD is to stop smoking. Smoking cessation can slow disease progression and improve lung function.
• Avoid Pollutants: Reducing exposure to indoor and outdoor pollutants can help minimize respiratory irritation.
• Stay Active: Regular physical activity can strengthen respiratory muscles and improve overall health.
• Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support immune function and overall well-being.
5. Surgery
For patients with severe COPD who do not respond well to other treatments, surgical options may be considered:
• Bullectomy: This procedure removes large air sacs (bullae) that form in the lungs due to emphysema, improving breathing.
• Lung Volume Reduction Surgery (LVRS): In this procedure, damaged lung tissue is surgically removed to allow healthier lung tissue to expand and function better.
• Lung Transplant: For patients with very severe COPD who have exhausted other treatment options, a lung transplant may be considered.
Recommended Products for Managing COPD
1. Inhalers: Essential for delivering medication directly to the lungs (e.g., Albuterol, Tiotropium).
2. Nebulizers: Useful for those who have difficulty using inhalers; they convert liquid medication into mist for easier inhalation.
3. Oxygen Therapy Equipment: Portable oxygen concentrators or tanks to maintain adequate oxygen levels.
4. Air Purifiers: HEPA purifiers to reduce indoor pollutants and allergens that may exacerbate symptoms.
5. Smartphone Apps for Health Management: Apps like MyCOPDApp help track symptoms and medication schedules effectively.
6. Nutritional Supplements: Omega-3 fatty acids or multivitamins that support lung health can be beneficial.
7. Exercise Equipment: Resistance bands or stationary bikes for low-impact workouts tailored to individual capabilities.
Conclusion
While there is no cure for COPD, a combination of medications, lifestyle changes, pulmonary rehabilitation, and supportive products can significantly improve quality of life for those affected by this condition. It is essential for patients to work closely with healthcare providers to develop a personalized treatment plan that addresses their specific needs and goals. Regular follow-ups and adjustments to treatment may be necessary as the disease progresses or as new therapies become available. By incorporating these strategies into daily life, patients can better manage their symptoms and enhance their overall well-being while living with COPD.
